Osteoporosis
Osteoporosis makes bones weak and brittle and usually shows no symptoms until a fracture happens. Osteoporosis-related fractures most commonly occur in the hip, spine, or wrist. The condition is very common: one in two women and one in four men over the age of 50 will have a fracture due to osteoporosis. Early detection and treatment can help protect bone strength, mobility, and independence.
When to see a doctor
If you went through early menopause, experience a fracture from minimal impact, notice a height loss, or have multiple risk factors for osteoporosis, schedule an appointment to discuss further evaluation.

Causes and Risk Factors
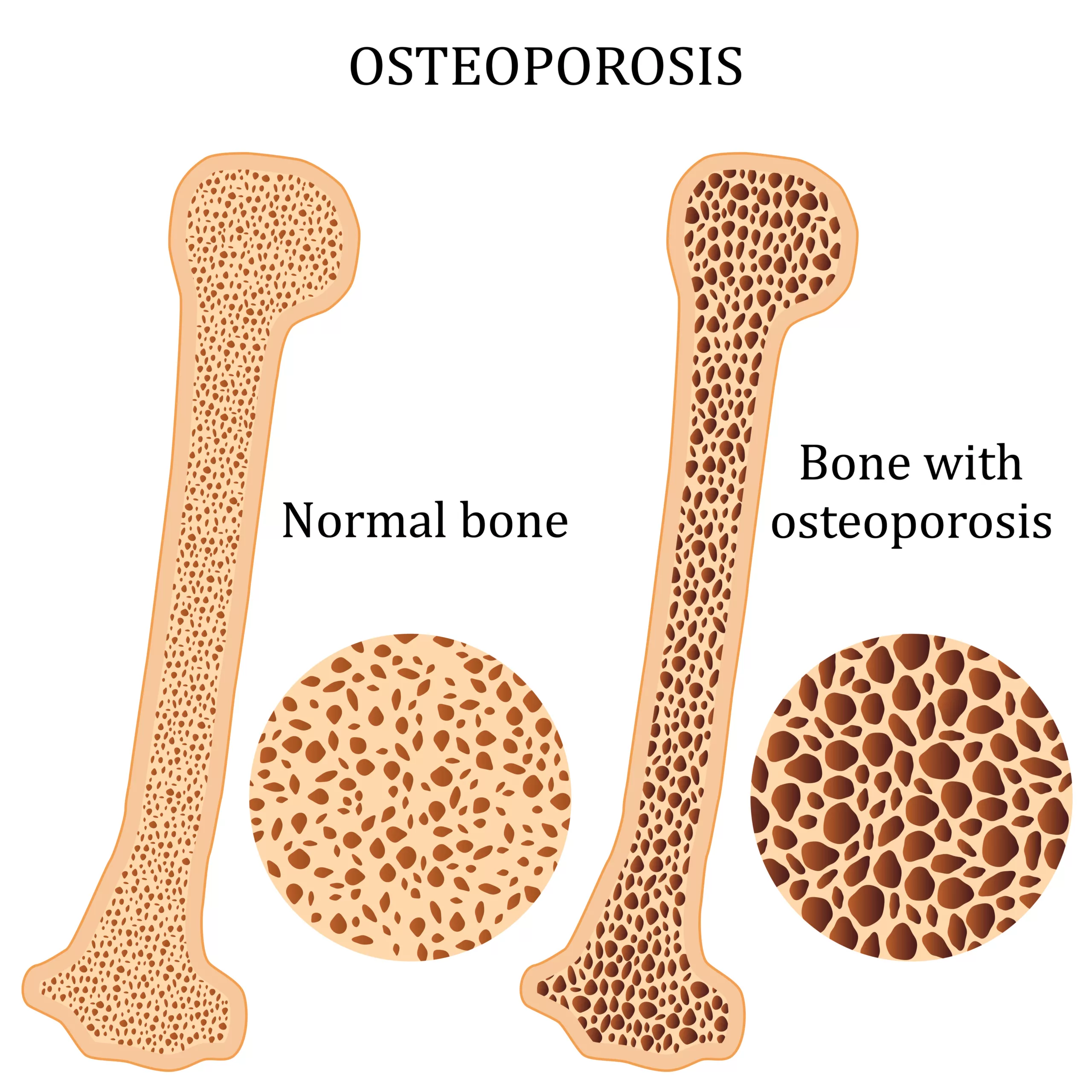
Bone tissue is constantly breaking down and rebuilding. During childhood and adolescence, the body makes new bone faster than it removes old bone, allowing bone mass to increase and reach its highest level by around age 30. After that, the rebuilding process slows, and over time more bone is lost than replaced. When this imbalance becomes significant, bones weaken and osteoporosis can develop, increasing the risk of fractures.
Risk factors include:
- Aging, menopause, or hormonal changes
- Long-term steroid use
- Race; white and Asian women are at higher risk
- Body size (thin boned), low body weight
- Poor nutrition, or vitamin D/calcium deficiency
- Family history, smoking, excessive alcohol
- Certain medical conditions or cancer treatments
- Lack of weight bearing exercise
Prevention
While osteoporosis cannot be prevented, healthy habits can help build and maintain strong bones throughout life. Steps to lower your risk include:
- Eating a balanced diet rich in calcium and vitamin D
- Engaging in regular weight-bearing and muscle-strengthening exercise
- Avoiding smoking and limiting alcohol use
- Maintaining a healthy body weight
- Taking steps to prevent falls, such as improving home safety and having regular vision checks
Building strong bones early in life and protecting them as you age are the best defense against osteoporosis.
Diagnosing Osteoporosis
Bone Density Test (DEXA)
Measures bone strength in a quick, painless scan to measure bone strength and track changes over time.
Fracture Risk Tools
Estimates future fracture risk and guide treatment decisions.
Lab Tests
May look for medical causes of bone loss and secondary causes.
Treatment Options
Osteoporosis treatment is tailored to each patient’s needs, focusing on slowing bone loss, improving bone strength, and reducing the risk of fractures. If your risk is not high for fracture, there are natural treatment options to slow the rate of bone loss.
Lifestyle changes: adequate calcium/vitamin D, weight bearing exercise, fall prevention
Medications: to rebuild the bone
Monitoring: periodic bone density testing (DEXA) to track your progress
Types of Osteoporosis
- Postmenopausal osteoporosis: most common form, linked to estrogen loss.
- Age-related (senile) osteoporosis: due to reduced bone formation with aging.
- Secondary osteoporosis: resulting from underlying conditions or medications (e.g., cancer treatment, endocrine disorders).
Osteoporosis may be silent, but its effects can be life-changing. At the Lowcountry Osteoporosis Center, we focus on early diagnosis, individualized treatment, and coordinated care to help you stay strong, mobile, and confident in your daily life.
The Lowcountry Osteoporosis Center Approach
We believe care should be personal and thorough. From your very first visit, we take time to understand your health history, lifestyle, and goals so we can create a plan that works for you.
Your care will be led by Katy Conner, MS, MSPAS, PA-C, who is passionate about helping patients protect and strengthen their bones. She has led the largest osteoporosis clinic in the Southeast US for the last 10 years. She has completed osteoporosis specific training through the National Bone Health Foundation. In addition, she has more than a decade of training in orthopedics and endocrinology so that she can treat your bone health with a multi-faceted approach. She will guide you through every step, from testing and diagnosis to treatment and ongoing support, so you always know what to expect in your care journey.
We also work closely with your other healthcare providers to ensure your treatment is well coordinated, effective, and focused on helping you stay active, independent, and confident in your daily life.

Katy Conner, MS, MSPAS, PA-C, Lowcountry Osteoporosis Center
Preparing for an Appointment
Before your visit, gather information that will help your provider create the best care plan for you.
- Any prior DEXAs or records of osteoporosis medications
- Bring a list of medications, vitamins, and supplements you take, including calcium and vitamin D
- Write down questions you want to ask
Frequently Asked Questions
Do men get osteoporosis?
Yes. Up to one in four men over 50 will break a bone due to osteoporosis, men should discuss risk factors and screening with their provider.
When should I get a bone density test?
Women 65+ should be screened; postmenopausal women <65 should be screened if they have risk factors. Talk to your provider about timing if you’re at risk.
What is a FRAX score?
FRAX estimates your 10-year fracture risk using clinical factors and bone density (if available). It helps guide treatment decisions.
How much calcium and vitamin D do I need?
Most adults need 1,000–1,200 mg/day of calcium and 800–1,000 IU/day of vitamin D; your needs may vary, ask your provider.
What exercises help?
Weight-bearing and strength exercises (plus balance work) help protect bones and prevent falls. Your provider can tailor a safe plan for you.
Are medications always needed?
Not always. Some patients do well with lifestyle changes; others need medication based on fracture risk and DEXA results. Treatment choices follow national guidelines.

