by Jessica Mason | Aug 25, 2025 | Uncategorized
When facing a cancer diagnosis, most people focus on treatments like chemotherapy, surgery, radiation, or immunotherapy. But another essential part of cancer care often goes underrecognized: supportive and palliative care.
These services help manage side effects, ease emotional burdens, and provide personalized support that improves comfort and quality of life. It’s important to understand what supportive and palliative care really mean—and how they can make a meaningful difference throughout the cancer journey.
What’s the Difference Between Supportive and Palliative Care?
- Supportive care includes a wide range of services designed to help patients manage the side effects of cancer and its treatment, cope with emotional challenges, and maintain well-being throughout the course of care.
- Palliative care is a specialized type of supportive care that focuses on relieving symptoms, pain, and stress related to serious illness. It’s appropriate at any stage of cancer, not just end-of-life, and is often provided alongside curative or life-prolonging treatment.
Both aim to improve quality of life for patients and families by addressing physical, emotional, social, and spiritual needs.
Why Supportive and Palliative Care Matter
Cancer doesn’t just affect the body; it impacts every part of life. Treatment can be physically taxing and emotionally overwhelming. Supportive and palliative care helps patients and families navigate these challenges with strength and clarity.
Benefits include:
- Relief from symptoms like fatigue, pain, nausea, anxiety, or shortness of breath
- Emotional support through counseling, social work, or spiritual care
- Guidance on nutrition, activity, and sleep to help patients feel their best
- Support for families and caregivers during treatment and beyond
- Improved communication and decision-making between patients, caregivers, and care teams
What Services Are Included?
Supportive and palliative care services can vary by practice and clinic, but often include:
- Symptom and pain management
- Palliative care consults
- Emotional support and counseling
- Spiritual care
- Advance care planning
- Psychosocial support
In addition to supportive and palliative care, many oncology practices offer a range of patient support services designed to enhance your well-being during and after treatment. These may include survivorship programs, nutrition counseling, social work and financial guidance, caregiver support, transportation assistance, and wellness classes. Together, they support your long-term quality of life and help you feel more confident and supported throughout your care. Ask our care team about the full range of services available—we’re here to help guide you every step of the way.
Who Can Benefit?
The short answer: anyone affected by cancer.
Supportive and palliative care are appropriate whether you’re newly diagnosed, in active treatment, recovering after treatment, or living with advanced cancer. These services are personalized to your needs and can begin at any point in your care, not just when symptoms become overwhelming.
All Parts of Your Care, Connected
Supportive and palliative care involves a coordinated team of experts working alongside your oncology team. This often includes doctors, nurses, social workers, dietitians, therapists, chaplains, and other specialists, all focused on your comfort, clarity, and quality of life.
Supportive and palliative care are not “extras”; they are essential parts of whole-person cancer care. They help ensure that your symptoms are managed, your voice is heard, and your emotional and physical needs are supported every step of the way.
If you or a loved one is navigating cancer, ask your care team about supportive and palliative care services available to you. You deserve care that supports all of you, not just illness.
by Jessica Mason | Aug 15, 2025 | Uncategorized
As summer temperatures peak and humidity lingers, cancer patients face unique challenges in the heat. Treatment and recovery can make it harder for the body to regulate temperature, stay hydrated, and avoid complications like heat exhaustion. With a few simple precautions, patients can stay safe and comfortable—even in the late-summer heat.
Why Cancer Patients Need to Be Extra Cautious in the Heat
Cancer and its treatment, especially chemotherapy, radiation, and some immunotherapies, can make it harder for your body to regulate temperature, stay hydrated, and fight infection. Certain medications may increase your risk of sun sensitivity, fatigue, or even heat stroke. And if your immune system is weakened, crowded summer events may increase your exposure to illness.
Simple Steps to Beat the Heat
- Stay Hydrated: this is especially important, and often more difficult, for cancer patients during the summer months. Both cancer and its treatments can increase your risk of dehydration due to a range of side effects like reduced interest in food and drink, nausea, vomiting, or diarrhea. Instead of waiting until you’re thirsty, try sipping water regularly throughout the day. Avoid caffeine and alcohol, which can dehydrate you further and worsen symptoms.
- Time It Right: if you want to get fresh air and exercise, try to go outside early in the morning or later in the evening when the sun is lower and temperatures are cooler. Avoid peak sun hours between 10 a.m. and 4 p.m.
- Dress for the Weather: choose lightweight, loose-fitting clothing and a wide-brimmed hat. Light colors can help reflect the sun’s rays. Don’t forget sunglasses that offer 100% UV protection to help protect your eyes—chemotherapy and radiation can make them more sensitive.
- Protect Your Skin: cancer treatments can make your skin more fragile or prone to sunburn. Use a broad-spectrum sunscreen with SPF 30 or higher, even on cloudy days, and reapply every two hours, or after sweating or swimming. Shade is your best friend.
- Listen to Your Body: heat-related illness can come on Symptoms like dizziness, muscle cramps or weakness, nausea, rapid heartbeat, or confusion could signal dehydration or heat exhaustion. If you experience any of these, move to a cool place and contact your care team right away.
- Keep it Cool Indoors: if you don’t have air conditioning at home, find public places with climate control, such as libraries, shopping centers, or designated cooling centers in your area.
- Maintain a Summer-Ready Emergency Kit: make sure you have access to water, snacks, any necessary medications, a charged phone, and contact information for your oncology care team.
When to Call Your Care Team
Let your doctor know if you:
- Experience any signs of dehydration or heat illness
- Have difficulty staying cool
- Notice changes in your skin (rashes, sunburn, peeling)
- Have persistent nausea, dizziness, or fatigue after being in the heat
Our care team can offer you or a loved one personalized advice tailored to your treatment and symptoms, and help you adjust your plans as needed to stay safe.
Enjoying Summer Safely
Even in the final stretch of summer, connection and joy are still possible with a little extra care. With the right precautions, cancer patients can safely enjoy the season’s final weeks. By staying aware of the risks and making smart choices, cancer patients can enjoy the sunshine without putting their health at risk.
For more guidance or questions about how your treatment may affect your end of summer plans, don’t hesitate to contact our team at any time.
by Jessica Mason | Jul 30, 2025 | Skin Cancer
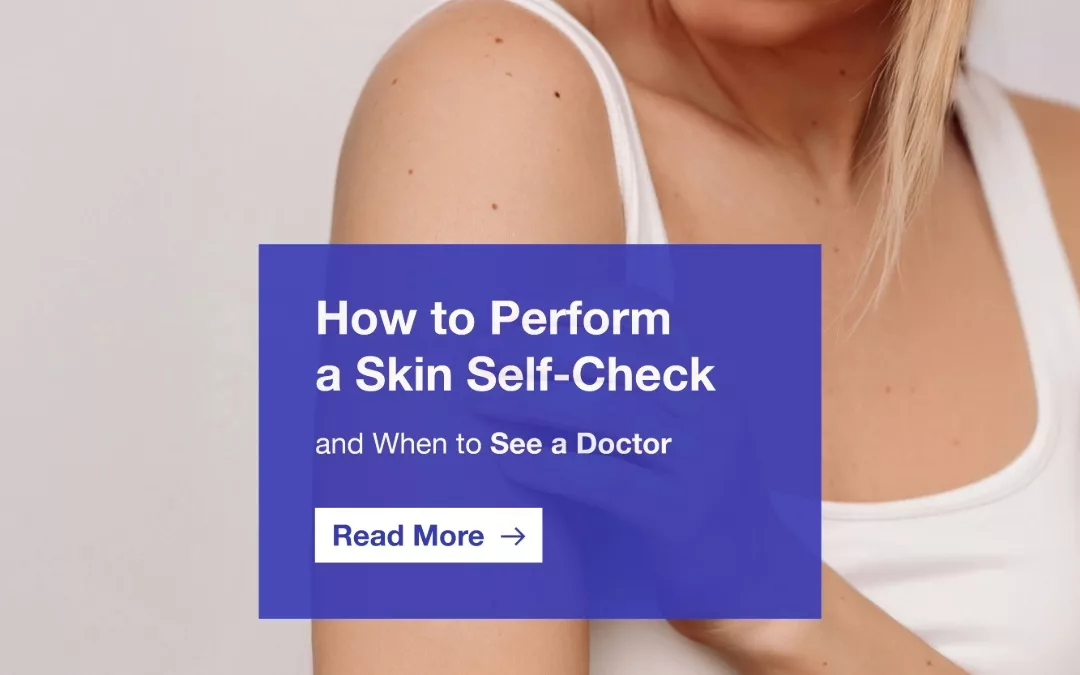
When it comes to skin cancer, early detection can make all the difference, and one of the most effective tools is a regular skin self-check. This simple at-home practice helps you become familiar with your skin so you can notice new or changing spots early, when treatment is most successful.
Whether you’re keeping an eye on an existing mole, noticing a new spot, or just being proactive, getting to know your skin, and what’s normal for you, can help catch potential problems before they become serious.
Why Skin Self-Checks Matter
Skin cancer is the most common cancer in the United States, with 1 in 5 Americans developing it by age 70. While routine visits with a physician are important, most skin cancers are found first by the person who has them.
Regular self-checks help you:
- Spot new or changing moles or spots early
- Track anything unusual between check-ups
- Know when it’s time to contact your healthcare provider
What to Look For: Use the ABCDE Rule
When you start your skin self-check, keep the ABCDEs in mind:
A = Asymmetry: one half doesn’t match the other
B = Border: edges are irregular, blurred, or notched
C = Color: varies in color, shades of brown, black, red, white, or blue
D = Diameter: larger than 6mm or about the size of a pencil eraser
E = Evolving: changes in size, shape, color, or behavior (itching, bleeding, etc.)
Also look for new growths or sores that don’t heal, spots that itch, bleed, or crust over, and any mole that feels different or stands out from the rest.
What You’ll Need and How to Do a Head-to-Toe Skin Check:
- Full length mirror
- Hand mirror
- Good lighting
- Chair or stool (optional, for checking feet or legs)
- A way to track any changes, this could be a skin map, photos, or a notes app
Follow these simple steps to examine your entire body:
- Start with your face, neck, and ears. Don’t forget behind your ears and along your hairline.
- Check your scalp. Use a comb or hairdryer to part your hair and check your scalp with a mirror or ask someone to help.
- Look at your hands and arms. Check your palms, the backs of your hands, between fingers, under fingernails, and both sides of your arms.
- Examine your torso. Look at your chest, stomach, underarms, and under your breasts if possible.
- Use a hand mirror to check your back and shoulders. You can also turn your back to a large mirror and use a hand mirror to see hard-to-reach areas.
- Check your legs and feet. Look at the fronts and backs of your legs, between your toes, the soles of your feet, and under your toenails.
How Often Should You Do a Skin Check?
Aim to check your skin once a month. It’s quick, easy, and helps you get familiar with your skin so you can notice changes more confidently over time.
When to See a Doctor
If you notice anything new, changing, or unusual, schedule an appointment with your doctor. Even if it turns out to be nothing, it’s better to be safe and catch potential issues early. You should also consider a professional skin check if:
- You have a history of sunburns or tanning bed use
- You have had skin cancer in the past
- You have many moles or a family history of skin cancer
- You notice something you’re not sure about
Skin self-checks are a simple but powerful way to protect your health. This July, and every month, take a few minutes to check in with your skin. And if something doesn’t seem right, don’t wait. Early detection can save lives.

by Jessica Mason | Jul 30, 2025 | Awareness Month, Skin Cancer
The sun is a powerful source of energy, but without protection, its ultraviolet (UV) rays, along with those from artificial sources like tanning beds, can cause lasting skin damage and significantly raise your risk of skin cancer, the most common cancer in the United States. July is recognized as UV Safety Month, a national observance that raises awareness about the dangers of UV exposure without protection and encourages habits to protect your skin every day.
While spending time outdoors has many benefits, being sun smart is essential to lifelong skin health. Understanding your risk and taking simple, consistent steps to protect your skin can make all the difference.
What Are UV Rays, Why Do They Matter, and What’s Link Between UV Exposure and Skin Cancer?
UV rays are a form of invisible radiation from the sun and from artificial sources like tanning beds that can damage your skin and eyes. There are two main types of UV rays that affect your body:
- UVA rays penetrate deep into the skin and contribute to premature aging, long-term skin damage, and sunburn. They’re present year-round, even on cloudy days, and can pass through windows.
- UVB rays are more intense and primarily responsible for sunburn. They directly damage skin cells and play a significant role in the development of skin cancer.
- In addition to harming your skin, UV rays can also damage your eyes, increasing the risk of cataracts, macular degeneration, and even cancers of the eyelids. Wearing UV-blocking sunglasses is just as important as protecting your skin.
The Link Between UV Exposure and Skin Cancer
Skin cancer affects 1 in 5 Americans by the age of 70, and UV radiation is the leading environmental cause. Here’s how it connects to the three main types:
- Basal cell carcinoma (BCC): the most common and slowest-growing form of skin cancer. It’s typically found on areas that receive frequent sun exposure, such as the face, ears, neck, scalp, shoulders, and back.
- Squamous cell carcinoma (SCC): often linked to chronic UV exposure over time. It can spread if left untreated and is most commonly found on the ears, scalp, neck, and hands—areas regularly exposed to sunlight.
- Melanoma: less common, but far more dangerous. Melanoma can spread quickly and become life-threatening if not caught early. It can appear on any part of the body, including areas not typically exposed to the sun, such as the soles of the feet or under nails. While UV exposure and sunburns increase risk, genetics and intermittent intense exposure also play a role. That’s why checking your entire body, not just sun-exposed areas, is crucial during a skin self-exam.
Who is Most at Risk?
While anyone can develop skin cancer, some factors increase your risk, including:
- Fair skin, light hair, or light eyes
- A history of frequent sunburns
- Use of tanning beds
- Family history of skin cancer
- A weakened immune system
- Spending a lot of time outdoors without sun protection
How to Protect Yourself
Practicing sun safety every day, especially in the summer, can significantly reduce your risk. Here’s how:
- Apply broad-spectrum sunscreen (SPF 30 or higher) every day, even on cloudy days
- Reapply sunscreen every two hours, or more often if swimming or sweating
- Wear protective clothing, wide-brimmed hats, and UV blocking sunglasses
- Seek shade when the sun is strongest (10 a.m. to 4 p.m.)
- Avoid tanning beds completely, they emit harmful UV rays
Protecting your skin doesn’t mean avoiding the sun altogether; it means being smart about your exposure. Incorporating habits into your routine like keeping sunscreen in your bag/car, setting reminders to reapply during long days outdoors, and encouraging loved ones to protect their skin, too can make a big difference right away.
When to See a Doctor
Early detection is key to successful skin cancer treatment. Perform regular skin self-checks and look for:
- New or changing moles or spots
- Asymmetry, irregular borders, multiple colors, or a diameter larger than a pencil eraser
- Spots that itch, bleed, or won’t heal
Use the ABCDE rule (asymmetry, border, color, diameter, evolving) to assess anything that looks suspicious. If you notice any changes, talk to your doctor.
This UV Safety Month, we encourage you to check in on your sun protection habits. Whether you are headed to the beach or running errands, daily precautions go a long way toward reducing your risk of skin cancer.

by Jessica Mason | Jul 21, 2025 | Awareness Month, Bone Cancer
Every July, we recognize Sarcoma & Bone Cancer Awareness Month, a time to increase understanding, support those affected, and elevate research for these rare and often overlooked cancers.
What is Sarcoma?
Sarcoma is a rare type of cancerous tumor that begins in the body’s connective tissues (bones, muscles, fat, cartilage, nerves, tendons, and blood vessels). It can occur anywhere in the body and affects both children and adults but is most often formed in the legs, chest/abdomen, arms, or head and neck.
Sarcomas are divided into two main categories:
- Soft Tissue Sarcomas: begin in muscles, fats, nerves, or tendons (angiosarcoma, desmoplastic small round cell tumors, etc.)
- Bone Sarcomas: begin in the bone itself (osteosarcoma, Ewing sarcomas, etc.)
Together, these cancers make up less than 1% of all adult cancers but are more common in children and young adults.
Most cancers are classified as carcinomas, which typically begin in major organs like the lungs, breast, or colon. These cancers often spread through the lymphatic system or bloodstream to other parts of the body.
Sarcomas, however, behave differently. They usually begin in connective tissues, like bones, muscles, or fat, and rarely originate in the organs. Instead of spreading through lymph nodes, sarcomas are more likely to travel through the bloodstream, often reaching the lungs, live, or in rare cases, the brain. This distinction is important in understanding how sarcoma progresses and how it’s treated.
Common Signs and Symptoms
While symptoms vary based on type and location, here are a few to be aware of:
- A lump or swelling (often painless at first)
- Pain in a bone or soft tissue that doesn’t go away
- Limited range of motion or joint function
- Numbness or tingling
- Unexplained fractures/pathological fractures
If any of these symptoms persist for you or a loved one, especially in combination, it’s important to consult a healthcare provider.
Why Awareness Matters
Because sarcomas are rare and often present with vague symptoms like swelling or pain, they can be misdiagnosed or overlooked. Early detection is critical, yet many patients face delays in diagnosis. Increased awareness can lead to earlier detection, better outcomes, and more attention to research funding.
Support for Patients and Families
A sarcoma diagnosis can feel isolating, but you are not alone. Throughout Sarcoma & Bone Cancer Awareness Month, we honor those impacted and provide resources to help:
Sarcoma and bone cancers may be rare, but the strength of the community is powerful. This month, and every month, we support patients, survivors, caregivers, and advocates to raise awareness and push for progress.